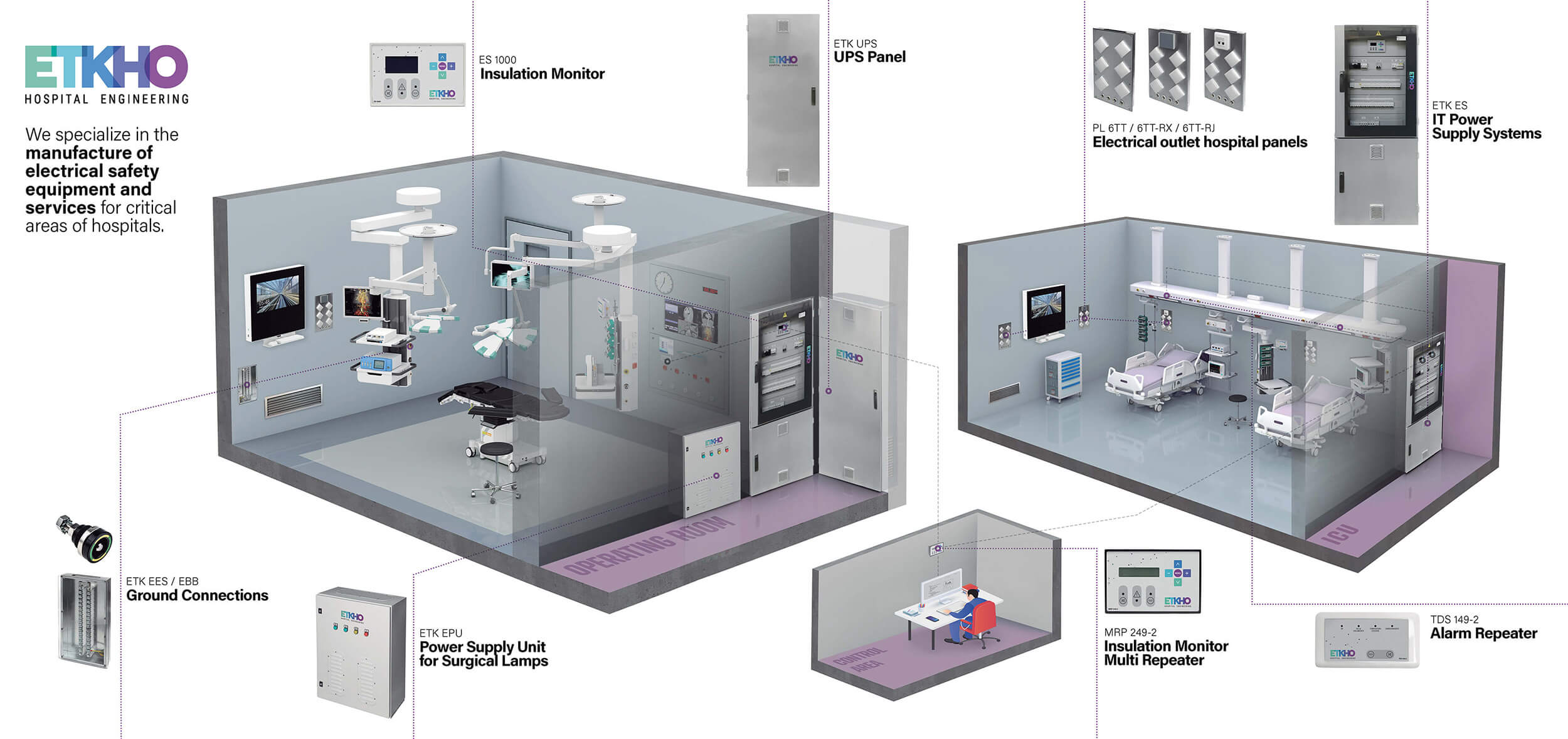
IT power supply systems
International and local standards require insulated voltage power systems for hospital critical areas.
We have a strong presence in hospitals throughout Spain and are steadily advancing toward international expansion. Our electrical safety systems are implemented in leading healthcare facilities, ensuring protection in critical hospital environments.

ETKHO Presence Area

ETKHO Project Details
We develop hospital electrical safety infrastructure solutions for
critical areas of hospitals: operating rooms, ITU or ICU.

International and local standards require insulated voltage power systems for hospital critical areas.

The medical insulation monitor continuously oversees the insulation resistance of IT medical systems.

Grounding sockets and connectors are essential in creating an equipotential ground connection, helping to avoid contact voltages in critical medical areas.

The Government of Spain has approved the Spanish Global Health Strategy 2025-2030 (EESG), a roadmap that reinforces the country’s international commitment to improve global health from an inclusive, sustainable and human rights-based approach.
The EESG was born in a context marked by the lessons learned from the COVID-19 pandemic, the climate crisis, the increase in inequalities and the threats to multilateral governance. With it, Spain becomes the fifth country in the European Union to adopt a specific global health strategy, aligned with the 2030 Agenda for Sustainable Development and the principles of equity, social justice, sustainability and international cooperation.

In the hospitality sector, the commitment to environmentally friendly architecture is no longer an option but an unavoidable necessity. The concepts of “sustainability” and “sustainability”, although derived from the same term in English -sustainable-, have been adopted in different ways depending on the country or region.
According to some authors, “sustainable” refers to something that maintains itself by its own means, while “sustainable” implies the support of external factors to maintain itself. Despite their etymological differences, both terms point to responsible planning that considers the present without mortgaging the future.
Construction, especially that of hospital buildings, is characterized by significant consumption of natural resources and energy. Healthcare infrastructures, which operate without interruption 365 days a year, require a different, more ecological and strategic approach.

In the hospital environment, where every second counts, electrical reliability goes beyond a simple technical requirement; it becomes a vital component of patient care. High-precision medical equipment depends on a safe and constant power supply, especially during critical procedures. However, the obsolescence of systems designed to ensure this continuity could pose an imminent risk.
Insulation monitoring systems are essential for the electrical safety of hospital facilities. These devices are designed to detect electrical faults in a timely manner and maintain operational continuity, even in the event of insulation failures. However, over time, these systems can become inefficient. False alarms, reading errors, or slow responses can jeopardize not only electrical safety but also the ability of medical personnel to respond effectively.

The World Health Organization (WHO) has designated the Center for Digital Ethics at Delft University of Technology (Netherlands) as its new Collaborating Center on Artificial Intelligence (AI) for health governance. This designation recognizes the center’s outstanding track record in research on responsible innovation and its leadership in integrating ethical values into the design of digital technologies.
AI has the potential to transform healthcare, improve clinical outcomes, and expand access to medical services. However, its implementation must be guided by sound ethical principles, evidence-based policies, and effective governance. The collaboration between WHO and TU Delft seeks to ensure that the adoption of AI in health is done in a safe, equitable, and responsible manner.
The TU Delft Center for Digital Ethics will play a crucial role in the WHO’s efforts to promote the ethical and responsible use of AI in health.

Today, healthcare is increasingly shaping up for a digital future, integrating technological advances that are transforming the way healthcare is delivered. Innovations such as social media applications, the Internet of Things (IoT), Artificial Intelligence (AI) and other digital tools are enabling doctors, nurses and other healthcare professionals to improve efficiency, make care safer and overcome physical barriers. These technological advances not only facilitate more accurate diagnosis but also empower more effective patient monitoring and management.
The World Health Organization (WHO) states that the future of healthcare will necessarily involve the implementation of digital health strategies.
In fact, the Pan American Health Organization (PAHO) defines the National e-Health Strategy as “the application of Information and Communication Technologies (ICT) to Health”, highlighting the crucial role of ICT for the collection, analysis and dissemination of health data. In this context, some countries have already implemented advanced systems for managing medical information, as in the United Kingdom, where digitization is key to ensuring a more efficient and accessible health service.

Five years ago, the world faced one of the greatest health crises in modern history. Since the WHO declared the pandemic on March 11, 2020, hospitals became the epicenter of an unprecedented battle: collapsing health systems, lack of resources, healthcare personnel at the limit and extreme pressure that tested the global response capacity.
Today, although the most critical phase is behind us and the pressure on hospitals has eased, the scars are still open. The pandemic left an indelible mark on hospital management, accelerating changes in infrastructure, protocols and medical technologies. In addition, the impact of long COVID continues to fill up surgeries, and the risk of new variants keeps health systems on alert.
Five years on, how has the hospital sector evolved? What lessons have healthcare professionals learned? This anniversary is an opportunity to analyze how the pandemic transformed healthcare and what challenges continue to shape the future of hospitals.